In our last post, we discussed what breast cancer is, what contributes to developing breast cancer, and some basic facts. In this post, we’ll be discussing Detection, Diagnosis, and Treatment.
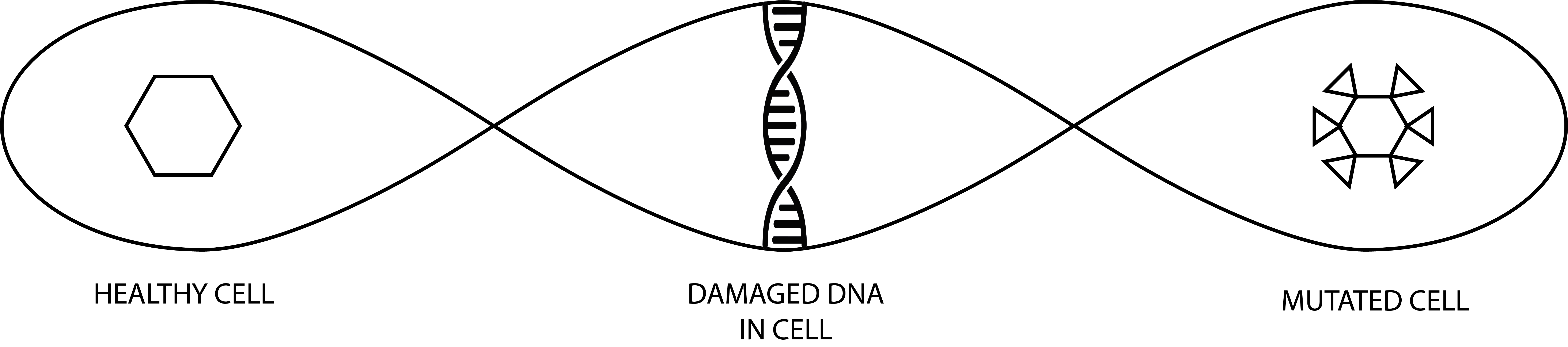
Just to recap, cancer occurs when cell growth takes an unusual path, building up old or damaged cells instead of casting them off. The resulting mass of tissue is a tumor. When it occurs in breast tissue, it is called breast cancer.
Detecting Breast Cancer
Early detection of breast cancer is crucial in the outcome. Since some of the symptoms are invisible, proper breast screening is very important. When detected early, the prognosis is very good.
Screening is a routine of tests and exams that physicians use to find disease in someone who doesn’t have any symptoms. In the case of breast cancer, routine screening can reveal areas of concern that are in the early stages and that can be more easily treated.
Early detection is the finding and diagnosing of a disease before symptoms are present.
Prognosis refers to the likely outcome from a disease. The size and how far cancer has spread outside the breast are the most important factors in predicting the prognosis.

Tools used to detect breast cancer
Breast self-exam
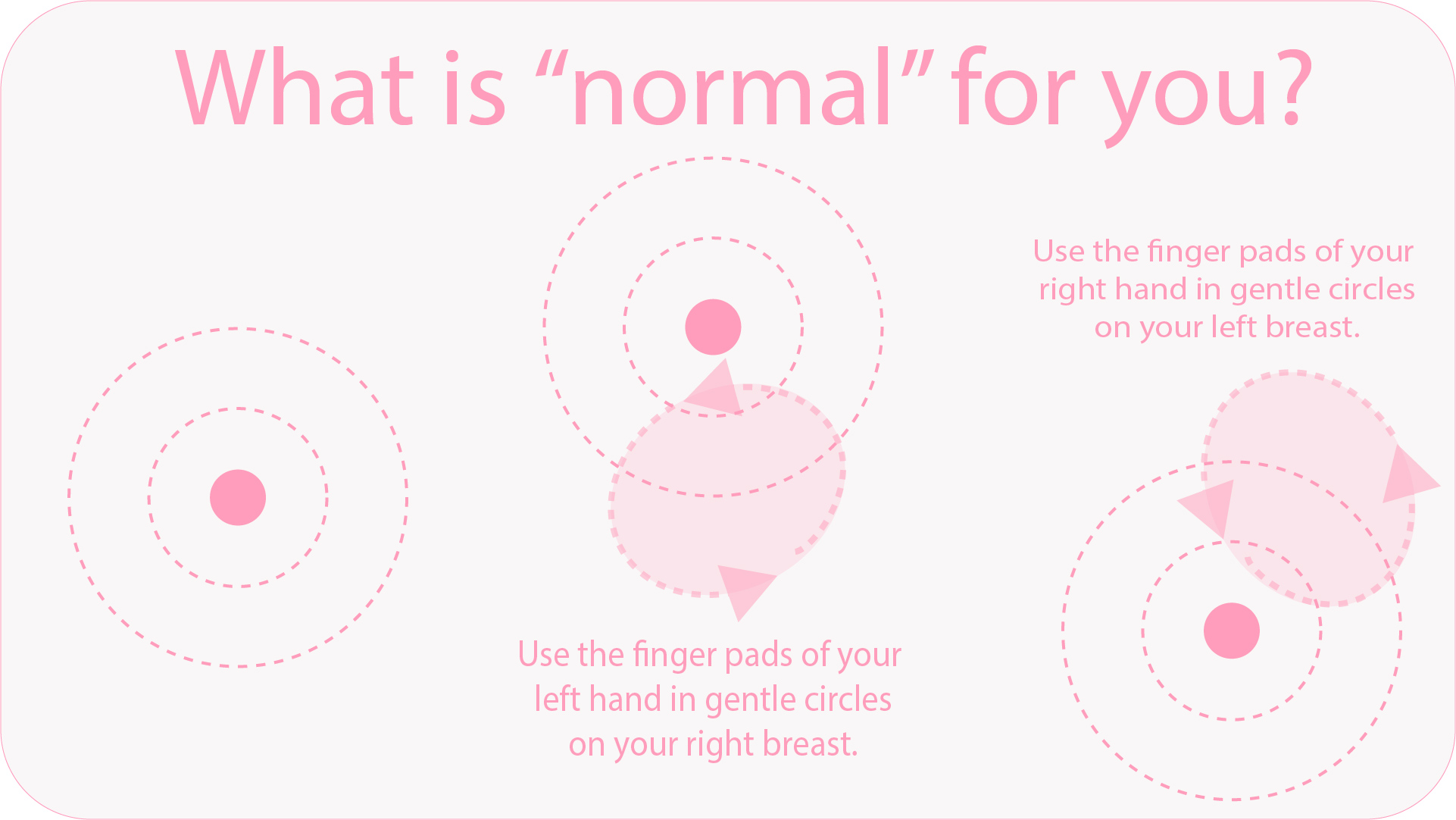
Your own fingers are your first diagnostic tool. Most healthcare professionals recommend performing a self-exam at least once a month. The goal is to know your own “normal” so well that your fingers will recognize even small changes so that you can alert your physician. Doing a breast self-exam is easy. Common ways to perform the exam include:
- Lying down—lie down on your back on a flat surface. In this position, breast tissue spreads out, making it thinner and easier to feel.
- In the shower—lather soap over your entire breast area so that your fingers glide smoothly over the skin.
General tips for doing the exam include:
- Use the pads, not the fingertips, of your three middle fingers. If you have a difficult time feeling with finger pads, use another part of your hand that is sensitive.
- Vary the pressure, using light, medium, and deep pressure in each spot before moving to another spot.
- Don’t hurry. Go slowly so that you have time to consider the perception of all the areas of your breasts.
- Imagine your breast like a pie, divided into pieces. Follow a pattern to examine every area thoroughly.
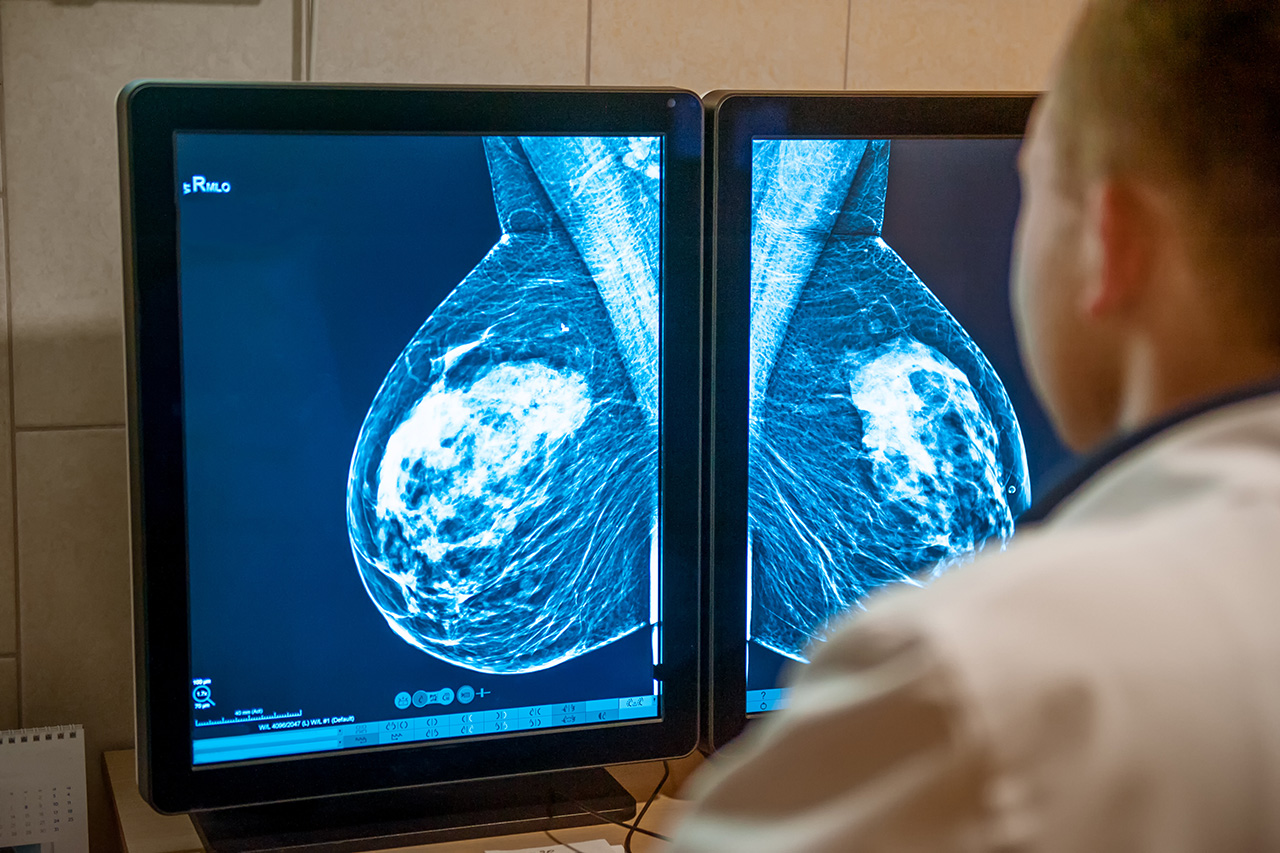
Mammogram
These low-dose x-rays are used to find breast cancer that your self-exam might miss. Mammograms can frequently detect breast cancer early, even before a lump can be felt.

Breast Ultrasound
Breast ultrasound uses sound waves and echoes which a computer can interpret as an image of the inside of the breast. Certain breast changes (such as fluid-filled cysts) can be difficult to see even with a mammogram, but an ultrasound can pick them up.
Breast MRI
MRI (magnetic resonance imaging) technology uses radio waves along with strong magnets that can make more detailed images of the inside of the breast. Because MRI can give “false positives” by revealing issues that are not cancerous, leading to other (perhaps unneeded) test such as biopsy, this imaging is not recommended for women at average risk for breast cancer. However, if cancer has already been diagnosed, MRI can pinpoint the size and location of a tumor.

Newer and experimental imaging tests
There are several newer tests that are not yet widely used to detect breast cancer. In the Netherlands, Radboud University Medical Center, is using AI (Artificial Intelligence) to help screen for cancer.
Artificial intelligence offers radiologists smart support in breast cancer screening. “The performance matches that of a good radiologist.”
— Ritse Mann, MD, PhD, head of breast imaging, Radboud University Medical Center, Nijmegen, the Netherlands
Others include:
- Abbreviated Breast MRI (fast breast MRI)—As with standard breast MRI, contrast (gadloinium) is given via IV before fewer images are taken.
- Digital Breast Tomosynthesis (DBT)—Also known as three-dimensional (3D) mammography, the machine takes many low-dose x-rays as it moves in a small arc around the breast. A computer program then assembles the images into a series of thin slices so that the physician can see the breast tissues more clearly.
- Nuclear Medicine Test—Called radionuclide imaging, this test utilizes a small amount of radioactive material (a tracer) which is injected into the bloodstream. The tracer then accumulates in cancer cells and can be imaged with a special camera.
- Contrast-Enhanced Mammography (CEM)—A contrast dye containing iodine is injected into the bloodstream. After a few minutes, two sets of mammograms that have different energy levels are taken to provide a clearer picture through the contrast.
- Elastography—part of an ultrasound exam that looks for differences in the elasticity of breast tissue. It is based on the assumption that breast cancer tumors are firmer and stiffer than normal breast tissue.
American Cancer Society Recommendations for the Early Detection of Breast Cancer
The American Cancer Society has screening guidelines for women at average risk of breast cancer, and for those at high risk for breast cancer. The following is a brief overview. We strongly recommend that women get familiar with their website.
Guidelines for women at average risk for breast cancer
If you fall into the category of average risk, the following will apply to you.
- You don’t have a personal history of breast cancer
- You don’t have a strong family history of breast cancer
- You don’t have a genetic mutation known to increase the risk of breast cancer (such as a BRCA gene)
- You did not have chest radiation before the age of 30.
If this describes you, the following schedule is recommended.
- Women between 40 and 44 have the option to start screening with a mammogram every year.
- Women 45 to 54 should get mammograms every year.
- Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
- All women should understand what to expect when getting a mammogram for breast cancer screening – what the test can and cannot do.
- Clinical breast exams are not recommended for breast cancer screening among average-risk women at any age.
Guidelines for women at high risk for breast cancer
If you fall into the high risk category, a yearly breast MRI and a mammogram are recommended. You are at high risk if:
- You have a lifetime risk of breast cancer of about 20% to 25% or greater based on family history
- You have a known BRCA1 or BRCA2 gene mutation based on genetic testing
- You have a first-degree relative (parent, brother, sister, or child) with the BRCA1 or BRCA2 gene mutation if you have not had genetic testing yourself
- You had radiation to the chest between the ages of 10 and 30
- You have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome or have first degree relatives with one of these syndromes.
The American Cancer Society recommends against MRI screening for women whose lifetime risk of breast cancer is less than 15%. Most women at high risk should begin screening with MRI and mammograms when they are 30 and continue for as long as they are in good health.

When the diagnosis is cancer
Nobody wants to hear that they have been diagnosed with cancer. It is a disease that strikes fear in the heart. However, not all cancer results in death; many women with breast cancer survive. What is important is the stage the cancer is currently in.
Cancer stages
After a cancer is found, your physician will order tests to see how big the cancer is and whether or not it has spread.
A lower stage (1 or 2) means the cancer is contained or has not spread much. A higher stage (3 or 4) means the cancer has spread from the original site to other areas of the body. Stage 4 is the highest stage. The cancer’s stage is crucial in determining the treatment.
Metastasis
Although cancer may have started in the breast, those same cancer cells can travel to other parts of the body via the bloodstream or the lymphatic system. Most of the free cancer cells will either die or be killed before they can lodge somewhere and start growing. However, some of them may reach another area and begin growing there. If they travel via blood, this could be anywhere in the body, especially organs. If it spreads through the lymphatic system, they will begin to grow in one or more of the lymph nodes.
Cancer that spreads is called metastasis and is said to have metastasized. If your doctor tells you that you have “advanced” cancer, it may not mean that the cancer has spread. Advanced cancer refers to cancer that cannot be completely eradicated, although the person with the disease can sometimes live a long life. Treating cancer appropriately is dependent on the diagnosis. Be sure you understand what your doctor means if you are told you have advanced cancer.

Treatment
All cancer treatments have benefits and side effects. Be sure your cancer team explains the different treatment options and what you can expect from each one. If you have questions, ask them. If you don’t understand, ask again.
Local treatments
When treatment affects the tumor but not the rest of the body, it is termed “local.” Both surgery and radiation for breast cancer are considered local treatments. Depending on factors such as the type and stage of the cancer, you may also need other kinds of treatments.
Systemic treatments
Drugs to treat cancer systemically can reach cancer cells nearly everywhere in the body. Drugs may be administered orally (in the mouth), by injection into a muscle, or by IV. There are different types of cancer-fighting drugs, including chemotherapy hormone therapy, target drug therapy, and immunotherapy.
Some final words
When treatments have been tried but don’t control the cancer, some people may want to weigh the benefits and risks of continuing to try new treatments. In fact, when cancer is advanced, some people may not want to be treated at all. This decision should not be made alone. It’s important to include your doctor in that decision, and in some cases, you may want to ask family members to help you make the decision. But in the final analysis, it remains your own decision. But remember, even if you don’t want treatment for the cancer, you can still get supportive care to help with pain or other symptoms.

